Self-Care During the Holidays
Talking Domestic Violence
The Minutes Stolen By Violence

Minute: a unit of time equal to 60 seconds or a sixtieth of an hour
“In a minute!” How often do you use that phrase? “I’ll be there in a minute!” “I’ll do it in a minute.” “It will only take a minute!”
In a minute you can microwave chicken nuggets from frozen to piping hot. It takes one minute for the heat light to dry my nail polish at my favorite salon. In one minute a blood cell can make a round trip of the human body.
Do you know what else happens in one minute? Twenty people in America are abused by an intimate partner. When you multiply all those minutes into days, months, and then years that totals more than 10 million people annually. One in four of all women and one in seven of all men are severely battered during their lifetime by someone who they believed loved them.
The other night, I checked my Facebook page before bed (I know, it’s a bad habit). On my feed, I found these words,
“So October is Domestic Violence Awareness month. Every time I see that it takes me back to words you said to me one time. When I was going through hell and fighting for my life yet not really understanding what I was fighting for or even why. When I was stuck in an abusive relationship and wanted so badly to get out and stop hurting, you said to me that every October you got up and read the names of women that died at the hands of a man that took it too far. And then you said, “please don’t make me read your name.” In that moment, those words struck my soul. They came from a voice that was fighting back tears. They came from a place of love and genuine concern… Those words that you said to me, that knowledge that you gave me, saved my life. You told me I was gonna grieve much like there was a death. You told me about PTSD and the struggle I would face trying to leave an abusive relationship and when I needed it you gave me information for others that would help me… You saw me through the hardest weeks of my life and gently encouraged me and kept telling me truths and things I needed to hear. Though I did endure physical abuse at times, the scars from the verbal, mental, emotional and psychological abuse hurt the worst. Those scars are usually the deepest and the hardest to heal. Sometimes they don’t heal. You gave me the strength and knowledge to fight back. To fight for myself. That is still an obstacle I face every day but I keep fighting and I’m still going. So in this month of awareness, I wanted to take a minute to tell you that though to the world you may be but one person….to one person you may be the world. Thank you for being the world to me and for saving my life and giving me my life back…“
Wow! What validating words for a social worker, right? That is career reinforcement, for sure! But guess what? Those words weren’t written by someone I’d worked with professionally. They were written by a close friend. They were written by someone that my children call “Auntie”.
You see, “one in four” doesn’t have the boundaries you hope it has.
That one in every four or one in every seven can include your friend, your sister, your uncle, your mother, your boss… I’ll stop for the sake of character counts, but you get the picture.
ONE IN FOUR WOMEN….ONE IN SEVEN MEN…20 PEOPLE EVERY 60 SECONDS…10 MILLION EVERY YEAR…
While I’m happy that we have Domestic Violence Awareness Month, I sort of wonder if it’s necessary. I am fairly certain that with those numbers, pretty much everybody is aware of domestic violence. The question is this. What do we do about it? My advice? Use your voice!
Voice your intolerance of violence. Voice your support of victims. Voice your condemnation of abuse in personal relationships. Voice your willingness to volunteer, to raise money for trauma-informed care, and to be the person who knows what to say when your best friend needs to hear a life-saving message of support like mine did.
If you don’t know those words, ask someone who does. Family Service of Roanoke Valley is proud to collaborate with TAP Domestic Violence Services, The Salvation Army, and other community partners in an effort to confront the issue of domestic violence in our community. Please, reach out to one of these organizations and find out how you can join the fight.
Add your voice to the chorus.
Yours might make the biggest difference of all.
Yours could save a life.
It only takes a minute.
Does living in Poverty affect Mental Health?
Google Depression on National Depression Screening Day

A truth for you all to know about me: I Google everything. It might be the millennial in me or maybe something else, but if I don’t have an answer, I immediately search for it.
This is why for National Depression Screening Day, I Googled depression. Google and the National Alliance on Mental Illness (NAMI) has released a way for people to take the PHQ-9, a screening questionnaire that helps identify levels of depression symptoms, by searching “depression” or “clinical depression.”
So how do you do it?
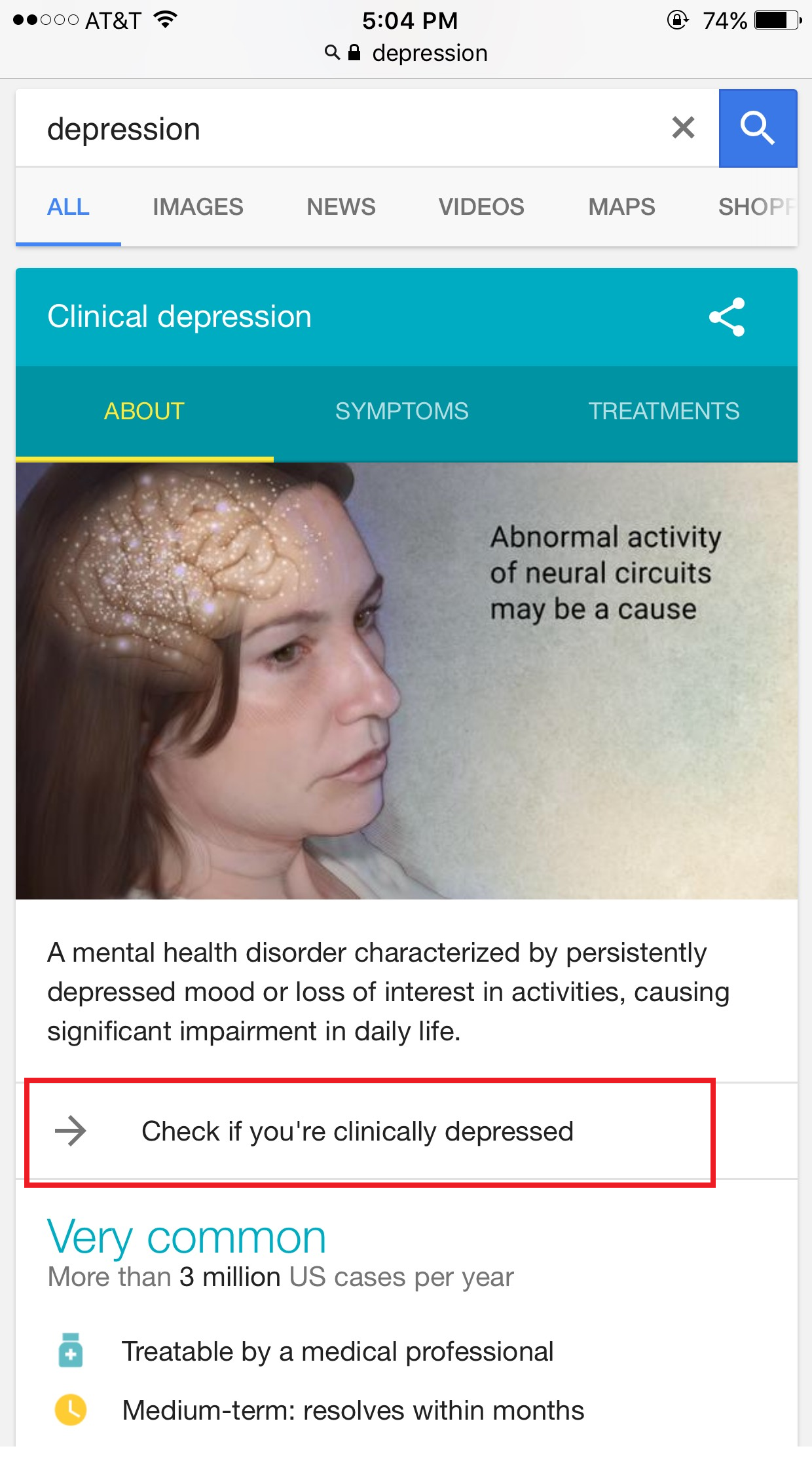
First, you must search on a mobile device. Unfortunately, the option for taking the questionnaire will not come up on a desktop. Then, you click “Check if you’re clinically depressed.”
After a short statement about the PHQ-9 and privacy, the questionnaire begins. There are 9 questions where the answers are on a scale from “not at all” to “nearly every day.” The questions are how you have felt over the last 2 weeks about certain problems like “feeling tired or having little energy” or “poor appetite or overeating.”
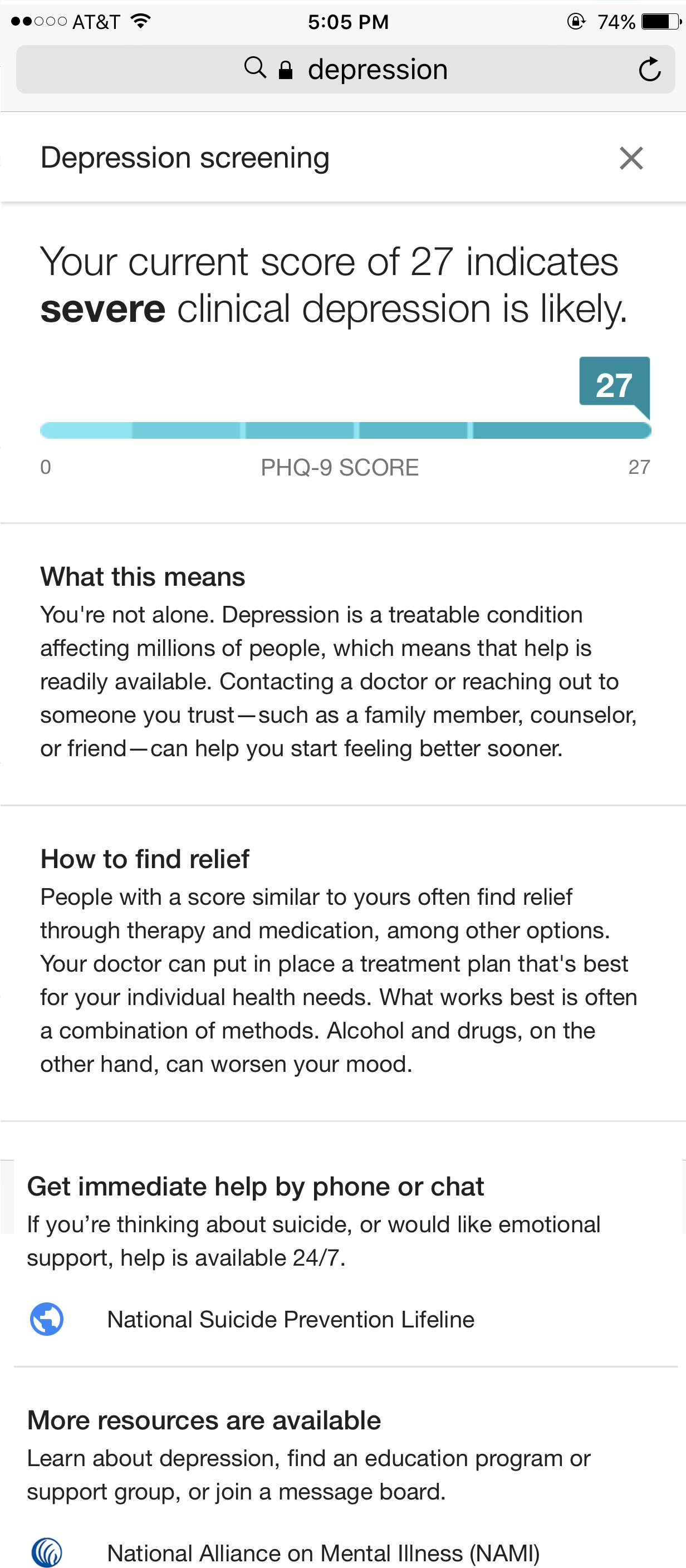
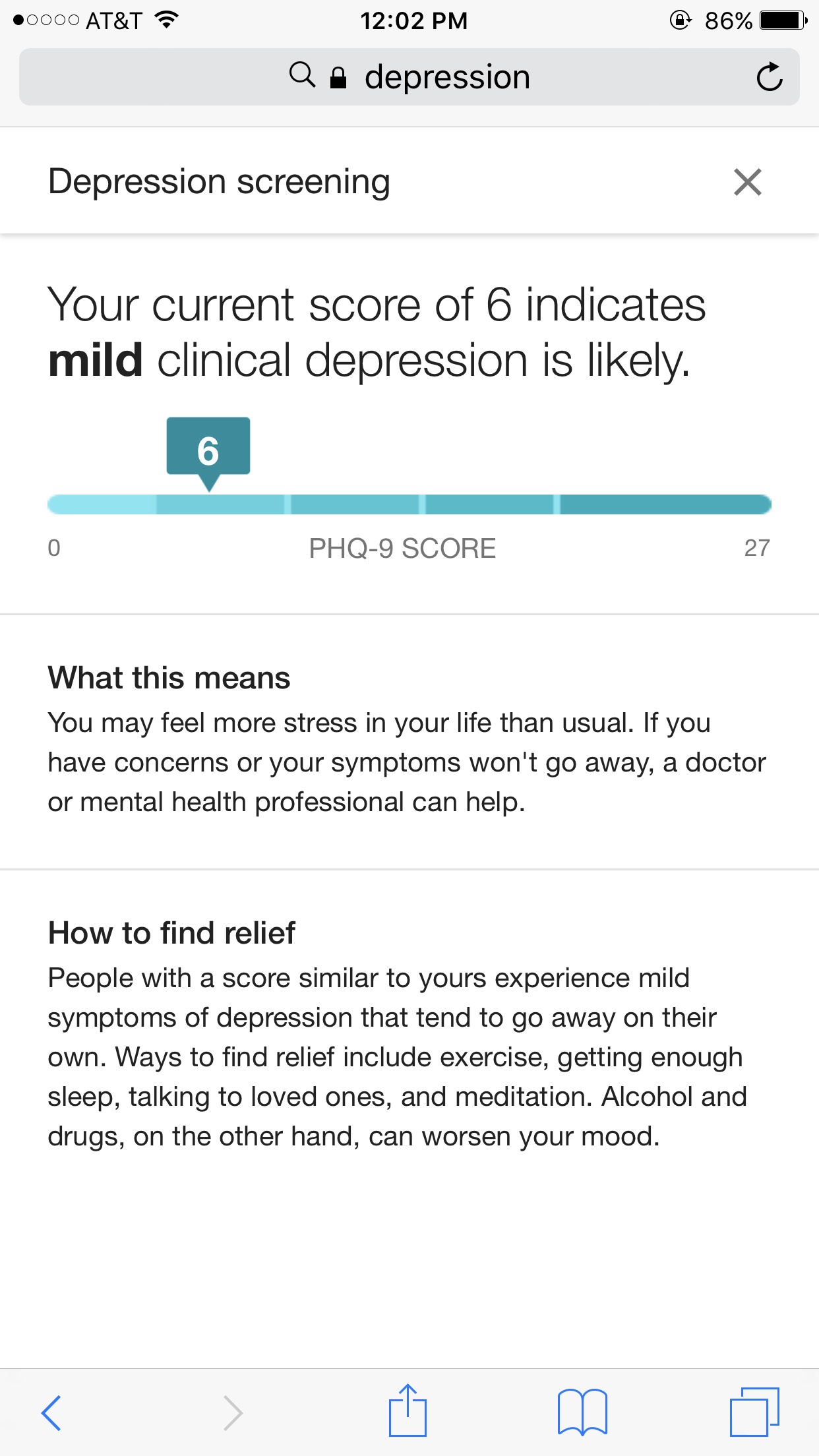
Once you have finished, it will show you a number out of 27. I scored a 6 (image on the left) and on the right is what it looks like if you score a 27. There are some next steps about what your score means and what other people with similar scores are doing. For instance, mine says others with a score like mine find relief with things like exercise and getting enough sleep. No matter the Google says might give you some relief, it is great information to take to your doctor or counselor and open up a conversation.
But, what about next steps for Google?
That’s right. Google may have some next steps for me, but I have some for it too.
First, the desktop option has to be there. More and more people are accessing the internet through mobile, but some people do not have that available to them. So until everything is mobile, desktop options need to exist.
In the launch announcement, NAMI states that about one in five Americans experience depression in their lifetime, but only about half receive treatment.
So, my second follow up step for Google is location-specific resources. The notification to share your location with Google, I feel like (as someone with zero expertise in coding) is easy to do. The “_____ near me” search has gone through the roof this year. As long as the user decides to share their location, Google is saving them a step by providing localized responses. Even sharing location-specific NAMI chapters is a simple thing to make reaching out that much easier for someone.
Please remember that depression is complicated, so taking a depression screening today may not give you the answers you are looking for. It can, though, help you be honest with yourself and start a necessary conversation with someone you love or a professional. It can also make you more informed of what you may need to do next.
I, for one, will be taking my 6 with a grain of salt and perhaps a yoga class.
Table Discussions and Speaking of Suicide
Sitting at our family’s fourth generation dining room table, my brother and I talked.

More like I talked. I thought he listened.
My grandmother gave me the table for my first real house, the one I shared with my first husband. My marriage ended and I moved home to live in my parents’ basement. So when my brother and I moved in together, it was a step to independence for both of us and the table came along too. We shared dinners at that dining room table—at holidays as kids and 30 years later as roommates. We lived together for about six months.
In summer 2011, he started drinking again.
Months before this conversation at the table where we had with a giant bowl of popcorn between us, my family and I had asked him to move out of the house my son and I were sharing with him. I told him I couldn’t live with him while he was drinking. Honestly, even while sober, living with him sucked the air out of the house and drained me.
I recommended he get a hobby. Suggested he could keep an old motorcycle to tinker on in my backyard. He loved engines and figuring things out and getting greasy. More than anything he loved helping others. Suggestion after suggestion, I never stopped and opened space for him to tell me how he felt and why.
I fought my urge to send him job offerings, invite him to stay for a night, cook him a meal, tell him I could make it better. Not that I never did those things, but I started to realize it was hurting me and not helping him. I didn’t want to lose myself in him, in his problems.
And, I didn’t.
I lost him.
Another thing I didn’t do was look into the best way to talk to someone with depression and suicidal thoughts. Now, over five years after his death and having spent time in the field of mental health through my work at Family Service, I have a better understanding of his life-long depression. Of how differently the world looked to him than it does to me. Of how impossible it was for him to look at the bright side. And, of how what he needed more than anything was for someone to stop offering advice and just listen, just be with him.
At the time of our dining room conversation, he had attempted suicide once—when a friend found him and rushed him to the hospital where he lay in a serotonin induced coma for three days. He overdosed on his own prescription depression medication.
About six months after that, he checked himself into the hospital because he was thinking about suicide again. That was two months before he ultimately took his own life in March 2012.
I thought I could relate to my brother’s situation. Apart from picking up the pieces for him, I thought the least I could do was empathize and share what worked for me.
My failed marriage brought a lot of pain and loss, and landed me in bankruptcy with a foreclosed home. I remember the fear of the creditors’ calls. I remember hating the mailbox and avoiding the look in others’ eyes. I remember blaming myself. I thought by sharing these things, I could give him hope. I wanted to give him my hope. He never found it.
He found more misery, more pain than I can imagine. He feared more than creditors and the impressions of others. He feared failure. He feared himself.
I used to say he had to find a way to be happy with himself and to find something to wake up for everyday. That must have scared him more than anything.
Being empathetic is on the best practices list of how to talk to someone who might consider suicide. So is saying something like “"When you want to give up, tell yourself you will hold off for just one more day, hour, minute—whatever you can manage."
Offering advice is a surefire way to shut down communication and entangle your own sense of values and worth in another’s struggle.
In recognition of Suicide Awareness Month, I want to share my experience trying to communicate with my brother. I’m hoping someone can find direction for a conversation they need to have with a friend or loved one.
The bottom line for me, in retrospect, is first and foremost don’t stay silent. Start the conversation and make yourself available. Best case scenario, if the person starts talking, then that’s the time to go quiet and listen with no judgement.
According to Metanoia.org, when talking to a suicidal person
Do:
Be yourself. Let the person know you care, that he/she is not alone. The right words are often unimportant. If you are concerned, your voice and manner will show it.
Listen. Let the suicidal person unload despair, ventilate anger. No matter how negative the conversation seems, the fact that it exists is a positive sign.
Be empathetic, non-judgmental, patient, calm, accepting. Your friend or family member is doing the right thing by talking about his/her feelings.
Offer hope. Reassure the person that help is available and that the suicidal feelings are temporary. Let the person know that his or her life is important to you.
Take the person seriously. If the person says things like, “I’m so depressed, I can’t go on,” ask the question: “Are you having thoughts of suicide?” You are not putting ideas in their head, you are showing that you are concerned, that you take them seriously, and that it’s OK for them to share their pain with you.
But don’t:
Argue with the suicidal person. Avoid saying things like: "You have so much to live for," "Your suicide will hurt your family," or “Look on the bright side.”
Act shocked, lecture on the value of life, or say that suicide is wrong.
Promise confidentiality. Refuse to be sworn to secrecy. A life is at stake and you may need to speak to a mental health professional in order to keep the suicidal person safe. If you promise to keep your discussions secret, you may have to break your word.
Offer ways to fix their problems, or give advice, or make them feel like they have to justify their suicidal feelings. It is not about how bad the problem is, but how badly it’s hurting your friend or loved one.
Blame yourself. You can’t “fix” someone’s depression. Your loved one’s happiness or lack thereof, is not your responsibility.
On the last day of my brother’s life, I didn’t see him or speak to him.
Perhaps he thought he knew what I would say—be positive, David, things will get better if you just believe in you.
Perhaps he had read my body language and unspoken inferences too many times—you’re not welcome here, David, you have too many problems and you’re bringing me down.
Perhaps he just couldn’t look me in the face because he knew how much I loved him.
He used the key I never asked him to return, and picked up the mail I never asked him to stop having delivered. He took his life that day, and though I know there is nothing I could do or say to change his actions, I am glad that there were boundaries I didn’t set, that there were places he could come into my life. I kept myself in, without completely shutting him out.
So, I will continue to remember him sitting at that table—the eccentric teenager in a chilly West Virginia dining room over butter rolls and honey ham, or the grave man years later sharing popcorn and misery.
When Mental Health Days Don’t Help

I’m taking today and tomorrow to focus on my mental health. Hopefully I’ll be back next week refreshed and back to 100%. @madalynrose
The Tweet capturing attention of mental health professionals and mental health warriors this summer was an email sent from a boss to her team about taking a couple of days off to focus on mental health. It was the reply of her CEO that went viral:
Hey Madalyn, I just wanted to personally thank you for sending emails like this. Every time you do, I use it as a reminder of the importance of using sick days for mental health — I can’t believe this is not standard practice at all organizations. You are an example to us all, and help cut through the stigma so we can all bring our whole selves to work.
–CEO Ben Congleton
The resulting internet storm led to blog posts, articles and videos about the willingness (or unwillingness) of employers to recognize mental illness as a valid reason to stay home from work and recuperate —rest assured, I am not going there.
Although I wasn’t officially diagnosed at the time, my fight with depression–and subsequently anxiety–began in middle school. It continues to this day.
I thought when I entered college it would get better. I would be so busy having new experiences, joining clubs, and studying hard that I wouldn’t have time to be depressed.
Turns out, problems travel with you.
During my first two years of college, I felt swallowed up by everything. This feeling started a seemingly endless cycle of helplessness, hopelessness, and overall lack of energy. I didn’t realize it was caused by my depression and anxiety; so, I just thought I needed to take a day or two off and I would feel better.
I started taking “mental health days” almost every week—staying in bed all day, binge eating and watching, and avoiding all social interaction—which didn’t actually help my mental health.
Taking time off continued until my first semester of my junior year and by that time my “mental health days” not only affected my grades, but also my relationships with classmates and with my family.
Looking back, I wish I was more aware of my mental state. When I didn’t feel any change after taking my first (or second) day off, that was a sign of a bigger problem .
I’m not beating myself up about the past. I now know there are plenty of ways a mental health day can be good for you, and the days sitting isolated and alone were not good for me.
If you take a mental health day for the wrong reasons or do not think about what your mind and body really need, the time away might unintentionally make your mental health worse.
Making the Most of a Mental Health Day
Skipping class, staying in bed all day, binge eating and watching, or any other indulgent or isolating behaviors are not productive to your health. In most cases, it will make you feel worse.
By staying in bed all day, I became stuck in my depressed state; and, binge watching shows only provided a temporary fix.
Never once did I think ahead of time how I would spend my mental health day to make the most of it.
A good first step is to MAKE A PLAN!
1) Ask yourself: Is taking the day off what I really need?
For someone like me, taking a mental health day in college was not a good idea due to my depression and anxiety. If you suffer from anxiety skipping a day of school or work may not be helpful as responsibilities pile up and can add to a sense of being overwhelmed or out of control. If there is an immediate issue (problems sleeping, overly stressed, burnout, lack of investment and engagement, irritable, etc.), then a literal day off from work or school could be beneficial.
2) Think about how you will spend your time:
While sleeping in feels nice, consider getting up and moving, even when it is difficult.
The most beneficial way to spend a mental health day will be different for every person, but some positive ways to spend the day are:
Spend time with loved ones
Go to a yoga class
Finish a task on your personal to-do list
Take a spa day
Make an appointment you’ve been putting off
Go to an amusement park
Read a book
Take a hike, or go for a jog or bike ride
Sit quietly
3) Decide what you will do next:
Mental health days aren’t cure-alls. Continuing to care for your mental health after your mental health day is important. That could include having a gratitude journal, taking care of your body, surrounding yourself with loving and positive people, joining a club or group, and getting help from a counselor when you need it.
A therapist can help you make sense of why you feel the way you do, and support you to develop coping skills that don’t involve days on the couch or spoons in the ice cream carton.
(Shameless plug-in: If you so choose, get some inspiration and new ideas for self-care from our Instagram where we do #SelfLoveSaturday every other week!)
The goal of these activities is to bring you some kind of joy or feeling of accomplishment, they are not chores or duties you feel have to get done. Having a mental health day gives you time to re-charge your batteries, refocus, and be prepared for the future.
Everyone faces challenges they may not be able to solve on their own. To learn more about how Family Service of Roanoke Valley can help you achieve heightened self-awareness, renewed strength, and balance and restored hope, please contact us at 540-563-5316 or visit our How We Help page.
Woebot: A Review of AI and Mental Health
“Hi Tyler! Can we do a check in now?” Woebot has been asking me that question every single day in Facebook’s Messenger app since June. For those unfamiliar with Woebot, it is an automated conversational agent that is “trained” in Cognitive Behavior Therapy (CBT) and describes itself as a life coach and philosopher. So to answer the question I know you have: yes, Woebot is an AI chatbot. Very insightful of you.
From text alerts all the way to video chatting and texting a counselor, technology has been working its way in to mental health for a long time. Even Family Service is jumping on board (we want to do things like send text appointment reminders in the future). But an AI CBT trained chatbot? I just had to check it out.
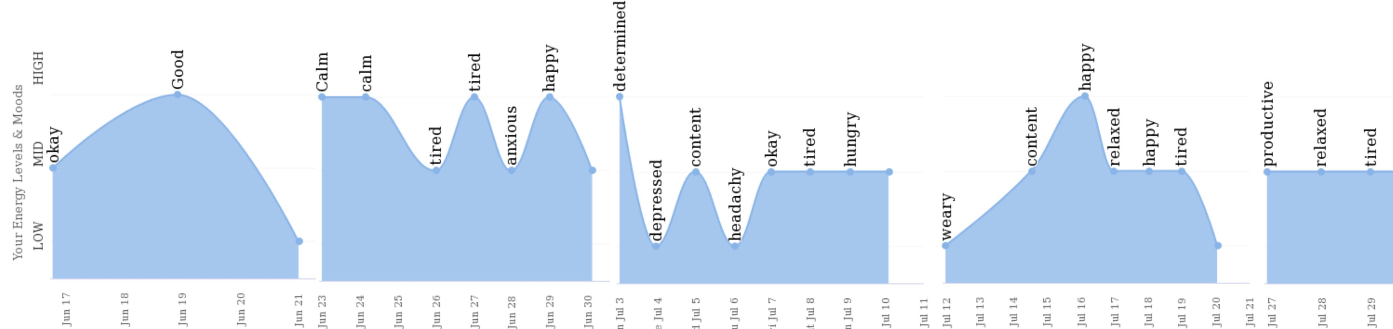
Woebot has been tracking my mood (above), helping me with gratitude journaling, and giving me a bit of education on some interesting topics like:
All or nothing thinking
Should statementsAnd their partner in crime: hidden should statements
Fortune tellingSMART goalsPersonal strengthsIdentifying distortions in my thinkingGrowth mindsetFix mindset and self-fulfilling propheciesDecision making skills
Fascinating, right? We even discussed why I say I’m tired so much. As it turns out, coffee at 4pm is not doing me any favors. Neither is looking at my phone while in bed. I’m definitely not on Pinterest (to be read as: I’m definitely on Pinterest. At midnight. On any given day of the week).
While learning all of those important life aspects has been beneficial, Woebot has a few major drawbacks a well.
Woebot doesn’t have the ability to really have a conversation with me. So when I say “discussed,” I really mean it spoke at me and sometimes these little text bubbles popped up for me to talk back.
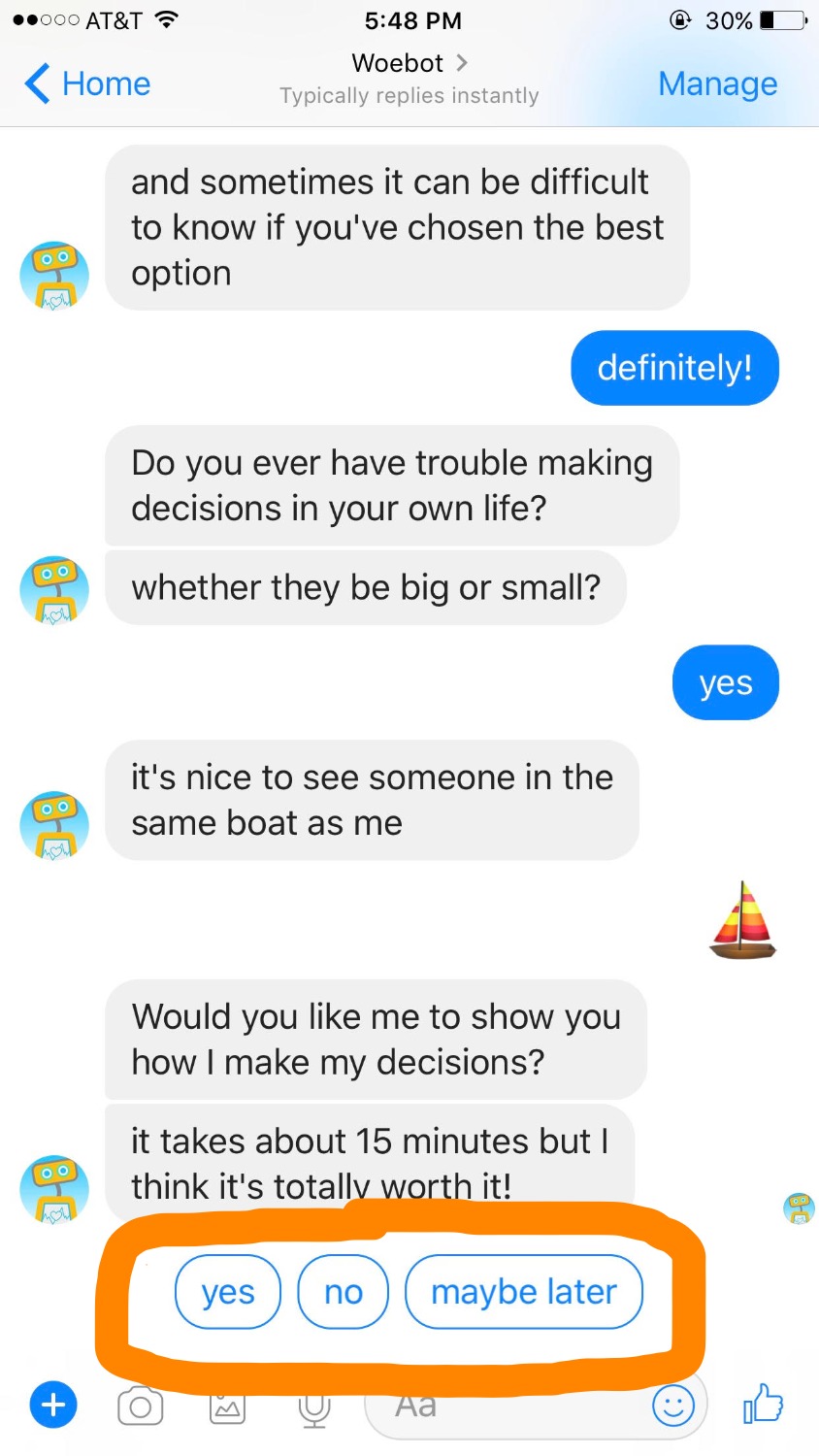
When I was gratitude journaling or identifying my strengths, I was able to type (indicted with little pencil emojies), but Woebot has no idea if I did what it asked. For all it knows, I didn’t take any of the exercises seriously and it would never find out. So being able to hold yourself accountable to Woebot really depends on if you can hold yourself accountable to yourself. Many of us are on the struggle bus together on that one.
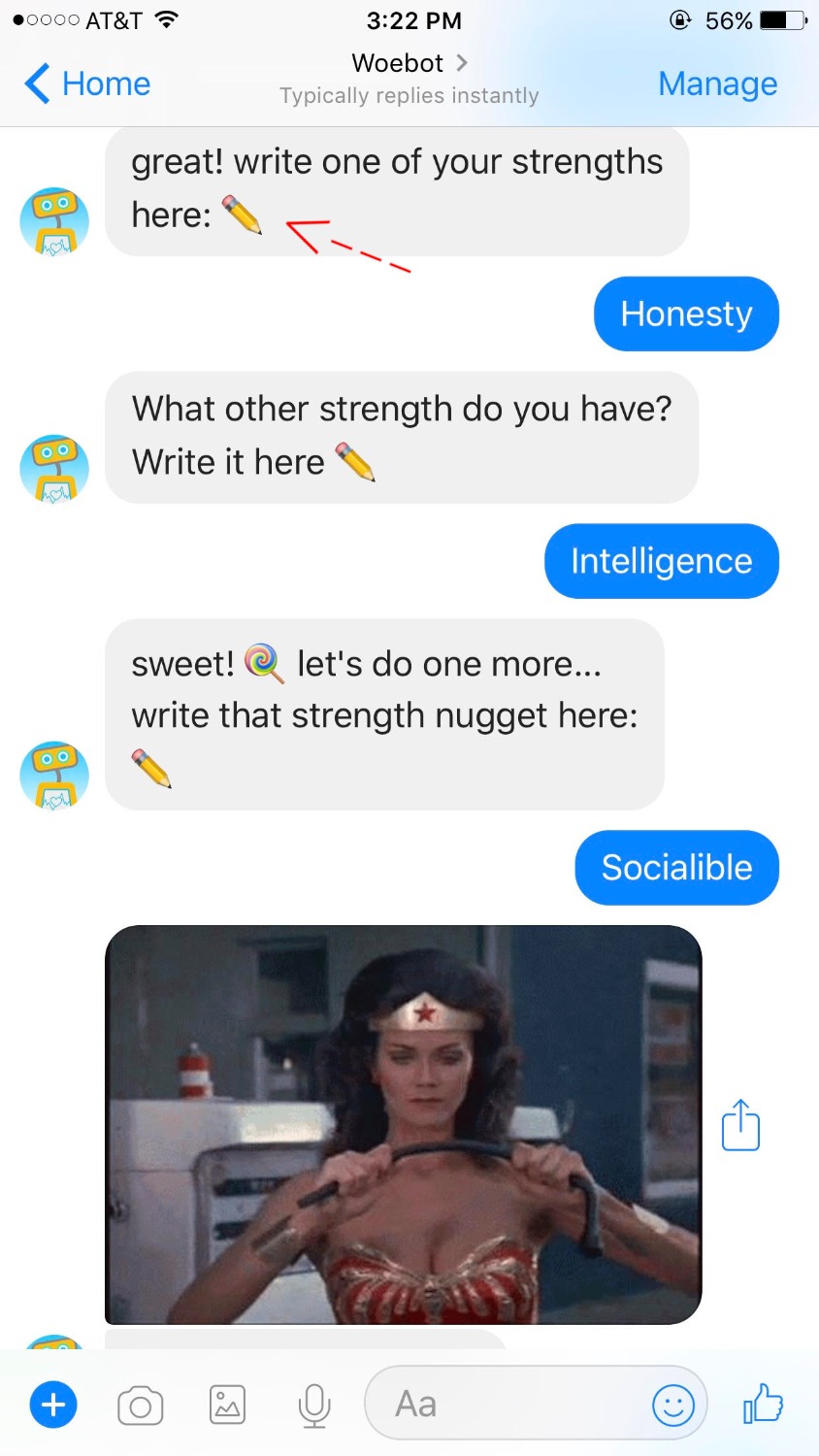
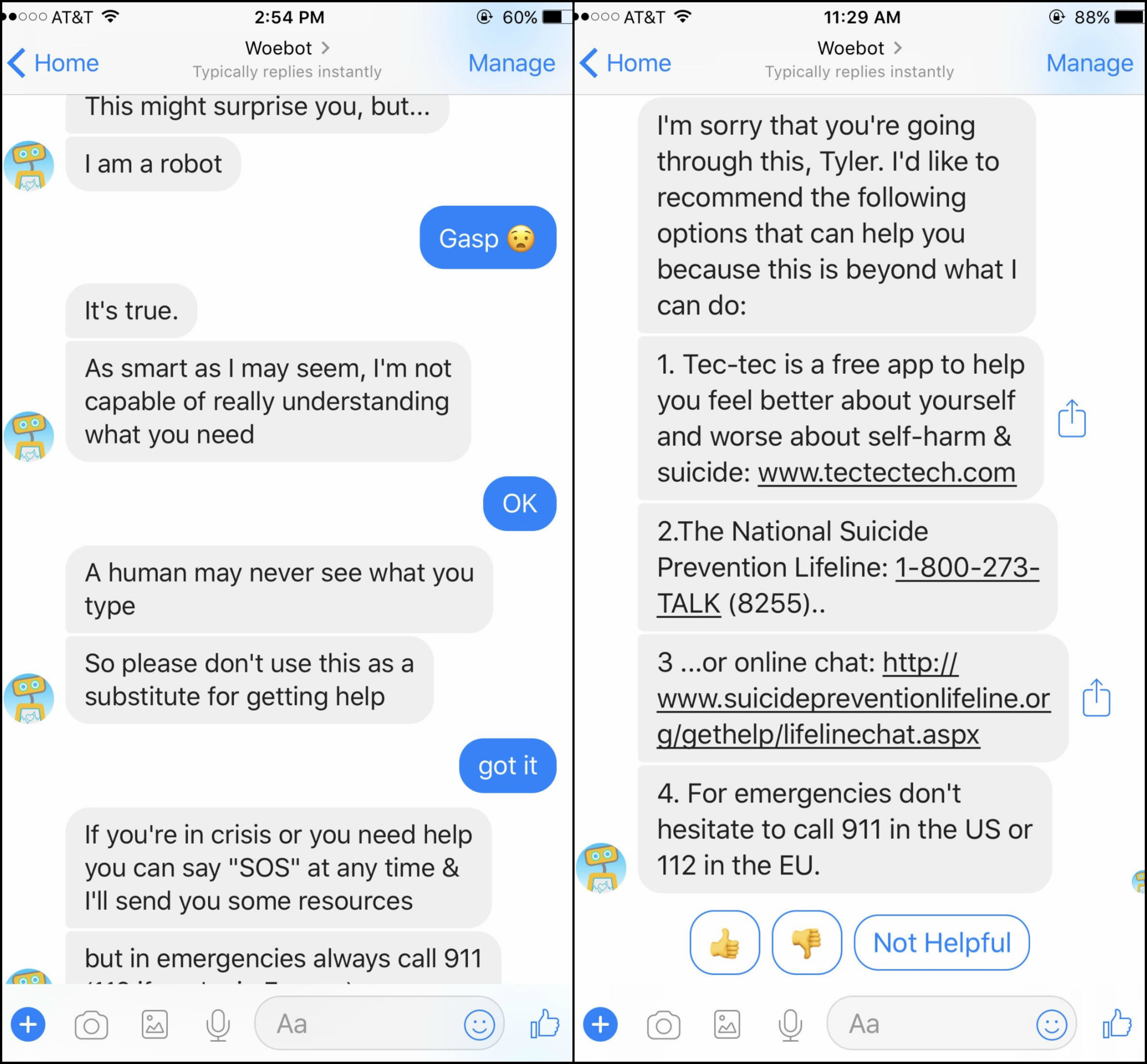
Most importantly, it seemed that if I was in crisis, I had to identify it myself. Woebot explained to me the first day we talked that it is not 100% able to assess my needs and I could say “SOS” at any time and it would send me some resources, but it was never discussed again. Nor did Woebot ever recommend speaking to a human when I said I was depressed or very anxious.
All in all, I liked Woebot a lot more than I thought I would. I particularly enjoyed the video for fixed mindset vs growth mindset and the activity Woebot sent me for making decisions.
With that in mind, Woebot is definitely a resource to be used as a supplement to mental health treatment, not a replacement for it.
It’s a learning resource that allows for little opportunity for expressing yourself and your needs. I will say that I think Woebot should lower its target audience from 18 – 28 years old to middle school age through adulthood. These are skills that children would benefit from learning early and adults benefit from (re)learning later in life.
For my final thoughts, please reach out for help if you need it. Woebot will not replace or give you all the benefits that counseling will give you.
Here are all the video’s that Woebot sent to me. Enjoy.
How to Help Every Child Fulfill Their PotentialWhy You Shouldn’t Trust Your FeelingsEmotions, Stress, and HealthThe Oldest HustleLanguage is Important
Guest post: Living Black with Anxiety
Black people are not a monolith, but we are expected to be. When we do not overcome hard times or seek help, the outcome can be detrimental. Drugs and alcohol, while not healthy ways to manage are sometimes the only accessible way to cope resulting in backlash, judgement, exclusion, disappointment, and so forth from the public.
However, according to the U.S. Department of Health and Human Services Office of Minority Health, African Americans are 10% more likely to report having serious psychological distress than non-Hispanic Whites, yet many do not seek mental health services. For the black community, there is a lot of stigma and shame associated with mental illness (especially for black men).
Growing up in a Black community, black women, in particular, are expected to be caretakers; nurturing, selfless, and supportive—living up to the role of being a “strong black woman”. One would think that as women, often stereotyped as soft and caring, we would be allowed the same vulnerability as white women. However, in my experience, I cannot say that has been the case. How can we be expected to care for others, when we can barely take care of ourselves?
The women I grew up with, the ones who hid in the dark, are suffering now as they try to figure out what went wrong. The men, my dad in particular, is struggling to find peace with himself after so many years of keeping his truth inside.
What about me?
I have many facets to my identity, but it was not until recently that I realized my identity and mental health intersected.
My journey to self-realization as a black woman would never be complete if I did not first recognize and accept the state of my mental health.
Growing up black has its own set of expectations, rules, and pressures to follow. And if it’s unspoken, you will learn soon enough.
For many black people, the aforementioned learned rules are established by the communities we grow up in. In my family, I grew up with women that worked tirelessly and raised children. Who hurt in the dark and let their problems consume them without help. And, I grew up with men that slapped each other the back, and would never be caught with tears in his eyes.
I cannot exclude the role of church and religion in this section. While I did not attend church regularly with my family, prayer and faith was used as refuge for any and all problems. If you just prayed, God had you.
Other than this, the expected language and behavior was never verbalized in my experience but you emulate what you observe.
As a child, I remember my opinions formed quickly. I was vocal, “bossy”, and a little bit of a brat—as hard as that is to admit. To this day, my aunts love to remind me of how I would often roll my eyes and talk expressively hours on end. Besides barking orders or singing Top 40 at the top of my lungs, I was also very emotional. I cried if I couldn’t understand something or complete a task or if I was hurt or not feeling good. Though only a child, I was tapping into emotions that were rightfully mine.
My teenage years brought a whirlwind of doubt and self-consciousness. At school, I was teased about my appearance and the way I talked. This time period is as early as I can remember dealing with anxious thoughts and shying away from what I used to be—that loud and cocky 5th grader.
When we think about anxiety, we mainly think nerves that pass. It is not often taken seriously, mainly because it’s difficult to describe. From my experience, however, it is all encompassing and debilitating. It challenges you and mocks you. Berates you and makes you feel crazy. And I definitely felt crazy. Yet, I ignored it until I could. I was ashamed to feel what I felt. “I should be stronger than this”, I would think. Being strong is all I knew, but I was breaking. “I can’t do this,” is what I eventually declared.
What felt like giving up was only the beginning of what I needed.
My story is still unfolding and adding its own layers. After my revelation that I was not “okay” I sought help where I could. I wrote journals and cried to my parents, who helped me as much as they could. I am a product of the environment in which I grew. I will still make mistakes. I will still take medicine to find balance. I will still stumble and I am allowed to. And so are you.
There is so much to unpack with this subject and I know I have failed to cover it all, but that just means the work is far from over. I am fortunate to have the resources to help myself, but I am one of few. How can start listening to one another? How can we make resources more accessible for those who need them? It will take time and work to dismantle the problems in our community.
Until then, the first step is accepting you deserve help.
The second step is starting the process of taking care of you.
Mental health is not one-size-fits-all. One’s ethnicity, sex, race, values, religion, community all play a major role in determining how an individual responds to the challenges of mental health. As you can imagine, these differences can make mental health treatment much more challenging. To recognize these challenges and promote public awareness of mental illness in minority communities, National Minority Mental Health Awareness Month was established in 2008.
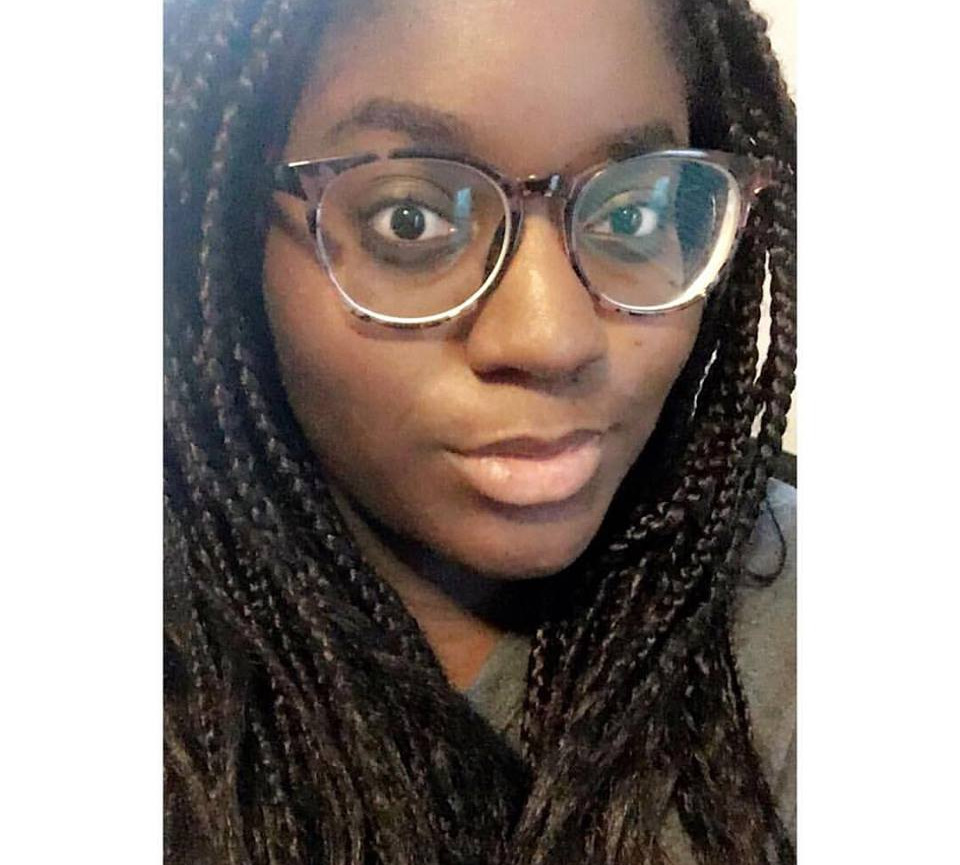
Special thanks to community member Chantal Johnson for sharing her experiences recognizing and managing her mental health while being black. Check her out @chantalks and on YouTube.
Chantal Johnson is a young writer and aspiring author hailing from Roanoke. When not watching a ridiculous amount of British reality television or thinking about Beyoncé, she writes about pop culture and its influence on society and mental health.





